A Race Against Time to Model COVID-19

(wan wei/Shutterstock)
As the United States braces for a potentially debilitating wave of COVID-19 patients over the next few weeks, the race is on to gather as much data about the spread of the virus, model its impact, and enact successful policies to minimize the number of people who will die.
Modeling the spread of diseases is a notoriously fickle affair. One of the key variables that researchers use is its RO factor, which is the number of people that a single sick person is likely to infect. For the novel coronavirus, that number is somewhere between 2 and 3, which is on par with regular influenza, but much lower than measles, which has an RO factor of 12 to 18.
In addition to the RO factor, researchers use data about the distribution of people and their travel patterns to predict how a pathogen will spread and who it will impact. Researchers with the Imperial College London, for example, used census data about the location of schools and workplaces to help flesh out its COVID-19 model for the United States and Great Britain.
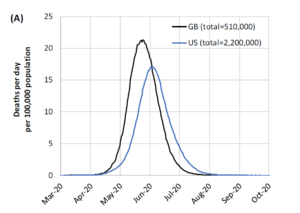
When the researchers put it all together, they concluded:
“In the (unlikely) absence of any control measures or spontaneous changes in individual behaviour, we would expect a peak in mortality (daily deaths) to occur after approximately 3 months (Figure 1A). In such scenarios, given an estimated R0 of 2.4, we predict 81% of the GB and US populations would be infected over the course of the epidemic.”
Imperfect data leads to imperfections in predicting the exact timing of the spread of the coronavirus, the researchers said. Nevertheless, the spread of the virus is expected to be broader in the US, and also to peak later, compared to Great Britain (GB), largely due to the US being larger and more susceptible to “distinct localised epidemics” in the individual states, the researchers wrote.
“In total, in an unmitigated epidemic, we would predict approximately 510,000 deaths in GB and 2.2 million in the US, not accounting for the potential negative effects of health systems being overwhelmed on mortality,” the Imperial College London researchers concluded.
Faced with the Imperial College London’s stark assessment, political leaders in both countries implemented many of the reports’ recommendations to slow the spread of the disease, including shutting down schools and universities, quarantining at home, expanding intensive care unit (ICU) beds in hospitals, isolating COVID-19 patients, and social distancing precautions, among others.
The worst is yet to come with COVID-19, as we’re still in the early stages of its predicted (exponential) spread. With that said, there is still a lot that we can do to fight coronavirus and dull its impact on our lives. People will live and die based on decisions that are made, and having the right data will be critical for making good decisions, particularly when it comes to distributing scarce resources, such as test kits, N95 masks, ICU beds, and ventilators.
Modeling Viral Response
As states and countries scramble to respond to the coronavirus, they’re struggling to match a limited amount of resources with rapidly changing needs. Forrester vice president and principal analyst Mike Gualtieri says artificial intelligence could help guide those decisions.
“For machine learning to be successful, we need a lot of data points about what we want to predict,” he tells Datanami. “So as people get sick, it would be … a worthwhile model to create.”
Eighty percent of the people infected with COVID-19 will have mild to moderate symptoms, and some will exhibit no symptoms at all. But a fraction of the infected individuals will need to be hospitalized, and a fraction of those will need to be admitted to the ICU and be hooked up to a ventilator to survive.
Predicting who will need a ventilator and who will survive without one is the type of problem that AI could help solve, Gualtieri says. “A model that predicted if someone came down with coronavirus, what is the probability that this person will recover without hospitalization, will recover with hospitalization, or will die” would be useful, he says.
“You hear what the risk factors are. But every person over 80 will not die,” he says. “Unfortunately, we’re going to have a lot of data about that. That would be a reasonable model to create, because then we can determine how to use the limited resources.”
With the tidal wave of COVID-19 cases expected to crest in the coming weeks, time is of the essence to create a useful model. “This whole thing could be over…by the time we had enough data,” Gualtieri says.
Improving COVID-19 Decisions
At this moment, it’s critical that politicians, healthcare professionals, and scientists from around the world come together to share what works, what doesn’t work, and craft a unified approach to battle COVID-19.
What would that look like? Harvard University professors Gary P. Pisano and Rafaella Sadun and Michele Zanini, the managing director of the Management Lab, gave us an idea in a March 27 story in the Harvard Business Review titled “Lessons from Italy’s Response to Coronavirus.”
The HBR authors make several recommendations for how to approach the viral pandemic. First, decision-makers need to recognize their cognitive biases. The coronavirus is an invisible foe that spreads in an exponential manner (with a devilish 14-day incubation period, no less), so it’s critical to act decisively early on, even if it appears to be an overreaction.
Getting in front of the virus is critical, and that requires anticipating where it will be next, not just responding to where it has already been. “An effective response to the virus needs to be orchestrated as a coherent system of actions taken simultaneously,” the authors write.
Speed is of the essence, so we need to look at what has worked, and what hasn’t worked, and adjust our approach – and do it quickly, the authors write. In particular, the HBR authors compared two regions of Italy, Lombardy and Veneto, which took very different approaches to combating the disease. Veneto had more testing early on, more contact tracing of potential cases, a stronger emphasis on home diagnosis, and monitoring of essential workers than Lombardi has, and its suffered a fraction of the deaths than its neighbor, they found.
Data also plays a critical role. “In an ideal scenario, data documenting the spread and effects of the virus should be as standardized as possible across regions and countries and follow the progression of the virus and its containment at both a macro (state) and micro (hospital) level,” they write. “Only by having good data at the right level of analysis can policymakers and health care practitioners draw proper inferences about which approaches are working and which are not.”
We can lean on time-tested approaches to devising a successful COVID-19 strategy, but it must be done quickly, the authors conclude.
“The difficulty in diffusing newly acquired knowledge is a well-known phenomenon in both private- and the public-sector organizations,” they wrote. “But, in our view, accelerating the diffusion of knowledge that is emerging from different policy choices (in Italy and elsewhere) should be considered a top priority at a time when every country is ‘reinventing the wheel,’ as several scientists told us.”
Related Items:
Can AI Find a Cure for COVID-19?
Tracking the Spread of Coronavirus with Graph Databases
How the Coronavirus Response Is Aided by Analytics